The amino acid tyrosine is often prescribed as an alternative strategy for treating ADHD, either alone (and often in the place of ADHD stimulant medications), or in combo with one or more medications for the disorder. But how effective is tyrosine really? Is it a valid ADHD treatment method, or just another theoretical supplement strategy that has only minimal positive effects on the disorder?
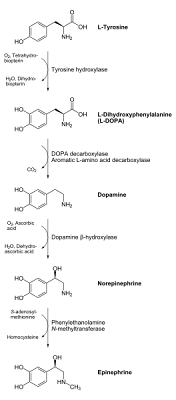
In the past four posts, we have examined the following metabolic pathway of tyrosine in the conversion process of this amino acid to the neuro-signaling chemicals dopamine, norepinephrine, and epinephrine (adrenaline) and the implications for this on the biochemical factors involved in the onset and treatment of attention deficit hyperactivity disorder.

- In part 1 of our series on ADHD and tyrosine supplementation, we did a quick overview of the above process, the connection between regional levels of these compounds listed above with regards to the neuro-chemistry of ADHD, and gave a general theoretical basis for tyrosine supplementation (based on its metabolic profile and some of tyrosine's biochemical products and pathways in the body). We also introduced the concept of the blood brain barrier, which is a biochemical barrier that controls the flow of chemical agents into and out of the brain. This blood brain barrier has numerous implications for drug design and therapeutics, and must be dealt with if we are to get the desired compounds, drugs and nutrients into the brain.
- In part 2 of the tyrosine and ADHD discussion, we looked at the enzyme Tyrosine Hydroxylase, and the dietary nutrients which were involved in making this enzyme run effectively. Some of the nutrient-based strategy were based on clinical trials, while others were more based on theory.
- Part 3 of the ADHD/tyrosine blog series centered around the merits of starting with tyrosine as a supplementation strategy vs. bypassing tyrosine and starting with the second compound in the above pathway, L-DOPA (also called Levodopa). L-DOPA is commonly used as a treatment agent in Parkinson's Disease (which has a moderate degree of overlap with ADHD as far as chemical happenings are concerned), but we investigated the pro's and cons of starting with this agent vs. starting with its precursor tyrosine for treating ADHD.
- and finally, Part 4 of the tyrosine postings zeroed in on the second major enzymatic step of the pathway, in which L-DOPA was converted to dopamine. This process is heavily dependent on a class of enzymes called aromatic amino acid decarboxylases, with the main enzyme of focus being a specific type called DOPA decarboxylase. In order for these enzymes to function, however, we discussed their dependence on a compound called pyridoxal phosphate (pyridoxal phosphate is an "active" form of Vitamin B6). We also looked at how competing amino acids and their products (namely the amino acid tryptophan and its product serotonin), actually share these enzyme systems and can interfere with the L-DOPA to dopamine conversion process and sabotage the effectiveness of the tyrosine-driven ADHD treatment strategy.
*Blogger's note: What follows is a lengthy explanation of why dopamine and norepinephrine are so important for ADHD, and how they interact with specific proteins called "transporters" or "receptors" to regulate their overall levels in key "ADHD" brain regions. If you are short on time, you may want to bypass this long explanatory section which starts and ends with a triple asterisk (***).
------------------------------------------------------------------------------------------------
***Begin explanatory section on dopamine and norepinephrine and ADHD
It is important to note, first of all, that this dopamine to norepinephrine conversion is not universal throughout all of the body, or even throughout the whole central nervous system. In many regions of the brain and nervous system, the chemical conversion process and metabolism of tyrosine "stops" at dopamine. However, in other key regions, the necessary enzymes exist to continue on with this conversion process to norepinephrine (and even beyond in some cases).
First, we need to address the all-important question, however: Why is the conversion of dopamine to norepinephrine important with regards to treating ADHD? To answer this question, we must look at some of the neuro-biology (and neuro-genetics) of some of the mechanisms which regulate dopamine and norepinephrine function in the brain:
We have hinted elsewhere that both dopamine and norepinephrine (namely imbalances of these two neuro-signaling agents) play a major role in the pathology of ADHD and its symptoms in most cases. However, it is important to note one very important thing here: many of the studies implicating dopamine and norepinephrine in the pathology of ADHD are often concerned more with the transport process of these two signaling agents into and out of neuronal cells, and are often less concerned with the overall concentrations of these two chemicals in the body or even the central nervous system.
Of course there is some degree of overlap (a vast overall deficiency of dopamine or its precursors, for example, would probably put one at more risk of having a deficit of this chemical in the key target areas of the brain), but we must get past the thinking that incorrectly assumes that if we just boost overall levels of these compounds across the board, then these chemical imbalances will just work themselves out. This is simply not the case, and unfortunately, in this blogger's opinion, many advocates of supplementation instead of medications often fail to address this all-important issue of the transport process.
Among the many different ways of transporting dopamine and norepinephrine in and out of the neuronal cells, we must look at two key players: the receptors and the transporters.
#1) The receptors:
The receptors (in a nutshell), are located on the outside of a cell (in this case, the neuronal cells in the brain), and are the place where signaling agents such as dopamine, norepinephrine, histamine, etc. essentially "dock" onto the cell. Proper functioning of these receptors is especially important with regards to disorders such as ADHD. We have even looked at some of the specific genes which code for these receptors, and have analyzed how certain genetic forms of these "receptor genes" are often associated with a higher likelihood of having ADHD.
For example, some of the earliest posts on this blog looked at specific genes that coded for dopamine receptors, such as the Dopamine D4 receptor gene (DRD4) and the Dopamine D5 receptor gene (DRD5) . The DRD4 gene is believed to be one of the most "heavily" influencing genes out there with regards to ADHD genes, while the DRD5 gene, while showing a somewhat weaker genetic connection to ADHD overall, seems to show a bit more of a specific connection to the inattentive component of ADHD (as opposed to the hyperactive/impulsive component of the disorder).
With regards to genetics and chemical receptors for the neuro-chemical norepinephrine, it appears that there are also some genes which may affect this norepinephrine-receptor relationship. There is some evidence for a specific gene called ADRA1A. ADRA1A is a gene located on the 8th human chromosome, and is believed to code for a specific receptor of norepinephrine. In fact, there are some implications that having a particular form of this ADRA1A gene may even influence the effectiveness of medications such as clonidine (which is a drug often used to treat hypertension, but is sometimes used "off-label" as an ADHD treatment medication. Clonidine has a different mode of action than the typical stimulants, but has found some success as a second or third level treatment method for certain types of ADHD).
It is important to note that several of the most common ADHD medications target (either directly or indirectly) these transporters, which influences the overall balance of dopamine and norepinephrine in and out of cells. In other words, if we want to truly replace drugs with nutrition for treating ADHD, we need to overcome this receptor problem (at least in theory). This is why (in the blogger's opinion) nutrition-based treatments often come up short, because while they may be able to influence production and overall levels of neuro-signaling agents such as dopamine and norepinephrine they are often nowhere near as chemically "potent" at modifying the transporter issues. If you're interested, an earlier post talked about some of the specific genes, receptors and transporters, and how some of these "ADHD genes" may even play a specific role on how we should dose ADHD medications.
#2) The transporters
Switching gears away from dopamine and norepinephrine receptors, we must also examine another important class of proteins which regulate dopamine and norepinephrine levels both inside and outside of neuronal cells. These are called "transporters". As their name suggests, these agents essentially go one step further in the process by shuttling neuro-signaling chemicals such as dopamine and norepinephrine both into and out of cells. In other words, these dopamine and norepinephrine tranporters also play a vital role in the process.
We can talk about these transporters all day (and we have, in other previous posts on this blog!), but for sake of brevity, I should just mention that specific genes for dopamine transporters (called the dopamine transporter gene or DAT), and for norepinephrine transporters (called the norepinephrine transporter gene or NET, however, it is also referred to by another completely different name: SLC6A2) both have been studied extensively with regards to their genetic influences on ADHD and related disorders. As mentioned earlier, these transporters often play major roles in medication responses, and may even be linked to co-occurring disorders in ADHD, such as bulimia, drug addiction, anxiety disorders, etc.
*In other words, these receptors and transporters (as well as the influences they carry on regulating neurochemical levels) are some of the main reasons why ADHD is believed to be so genetically influenced.***
-------------------------------------------------------------------------------------------------
***End explanatory section on the importance of regulating dopamine and norepinephrine levels in ADHD. The rest of the post is concerned with the dopamine to norepinephrine conversion process, and starts immediately below:
Here is a chemical representation of the dopamine to norepinephrine conversion process (don't worry if you're not a chemist, just look at some of the names of the compounds, enzymes and nutrients involved in the process, we will discuss all of these in thorough detail below):

From the above picture, we should note the two main components which need to be addressed in the dopamine to norepinephrine conversion process:
- The enzyme Dopamine Beta Hydroxylase, and
- The nutrient ascorbic acid (aka vitamin C), especially with its regard to oxygen (O2), as depicted above.
*Please note: It is important to note that oxygen is required for this step to work, as an oxygen atom is transferred from O2 to the dopamine molecule. In order for this chemical conversion to work, however, another agent (vitamin C) is required. This is where ascorbic acid (vitamin C) comes in:
Ascorbic Acid (vitamin C): We mentioned vitamin C in an earlier post, in that it can play a "helper" role in the conversion of tyrosine to L-DOPA, a process which utilizes the enzyme tyrosine hydroxylase. Tyrosine hydroxylase is dependent on iron, but the efficacy of the enzyme requires iron to operate in the "reduced" form as opposed to the "oxidized" form (the reduced form has iron in a "+2" positively charged state, and in the "oxidized" form, iron exists in the even more positively charged "+3" state. In nature how positively or negatively charged a certain element is can have drastic effects on its biological function. In the case of the tyrosine hydroxylase enzyme, and the metabolism of tyrosine, this is no exception). Much of this "helper" role of vitamin C was due to the ability of the vitamin to keep the iron in the desired "+2" state. Some studies have found this tyrosine hydroxylase enzyme to be significantly compromised in vitamin C deficient states (as in scurvy).
However, while tyrosine hydroxylase the enzyme Dopamine Beta Hydroxylase appears to be even more heavily dependent on vitamin C, as mentioned in an earlier blog entry titled: 10 Ways Vitamin C Helps Treat ADHD Symptoms (this was mentioned in point #9). For the conversion process of tyrosine to L-DOPA, much of vitamin C's usage was due to its antioxidant status, but for this dopamine beta hydroxylase enzyme, which is used to convert dopamine to norepinephrine, vitamin C is used more of as a "co-factor" or "helper" to the enzyme.
As mentioned above, vitamin C must be "sacrificed" to get the oxygen atom from the O2 molecule and onto the dopamine molecule to convert it to norepinephrine. The end result of this "sacrifice" is a different oxidized form of the vitamin, which is known as dehydroascorbate.
This brings up another important point. We have seen in the past how vitamin C is often an "altruistic" agent in ADHD treatment, in that it frequently sacrifices itself for the well-being of other nutrients of importance to ADHD. For example, we've spoken at length about the problem of oxidation of omega-3 fatty acids (since omega-3 supplementation is a common ADHD supplementation strategy, this damaging oxidation process can be quite severe if not controlled for), and how vitamin C can help in preventing omega-3 oxidation in ADHD treatment cases. Vitamin C often helps "recycle" other antioxidants such as vitamin E (which is much more fat-soluble than vitamin C, so it is often recommended for antioxidant treatment strategies for ADHD that vitamins C and E are used in tandem).
Please note, then, that since vitamin C is used in the dopamine to norepinephrine pathway, and that it is essentially "lost" in the process (unless it is returned to its native ascorbic acid form by another antioxidant, such as glutathione), it is crucial that we maintain adequate levels of vitamin C. Furthermore, since vitamin C is a water soluble vitamin, it gets removed from the system quite easily. Therefore, it is imperative that we maintain adequate pools of this vitamin through diet or supplementation. A rough estimate of daily vitamin C requirements can be found here.
However, since toxicity is rarely an issue with vitamin C (see the upper limits of the vitamin here, and note how much of a ceiling there is between the recommended levels and the upper limit), going slightly higher (i.e. 2 times the recommended amount) is rarely a problem. Therefore, this blogger personally recommends that since the vitamin is useful in at least 2 different parts of the tyrosine to dopamine and norepinephrine conversion process (involving both the tyrosine hydroxylase enzyme for the conversion of tyrosine to L-DOPA and the dopamine beta hydroxylase enzyme-driven conversion of dopamine to norepinephrine), those wishing to try tyrosine supplementation for ADHD should maintain adequate (if not slightly higher than "adequate") levels of the vitamin.
We will wrap up our discussion of tyrosine supplementation for treating ADHD in the next few blog posts. We will look briefly at the norepinephrine to epinephrine conversion process, but focus more on some of the potentially harmful side-products of tyrosine metabolism, including the potential buildup of the pro-inflammatory agent homocysteine. Finally, we will finish with a final post on the blogger's thoughts on the whole process, recap the different nutrients needed to optimize enzyme function for overall tyrosine metabolism, and look at possible ways in which, instead of being used completely in isolation, tyrosine supplementation could also be used as an adjunct or accessory treatment to common ADHD medications, possibly optimizing their function and improving their effectiveness in treating ADHD and related disorders.




 In our first post on
In our first post on